Maximizing the Care Team During Virtual Visits
This session focuses on learning and applying new virtual workflow strategies to engage your entire care team. The session was held live during Telehealth in a Post-Pandemic Era: Sustainable Approaches to Support Integrated Care – Part 2, held on September 29, 2021.Evidence Based Practices Workshop 3 Problem Solving Therapy
Problem-Solving Therapy (PST) is a form of therapy that provides people with tools to identify and solve problems that arise from life stressors that can have a negative impact on their day-to-day lives. Its aim is to improve individuals’ overall quality of life and can be used to treat depression, among other conditions. It is based on a model that takes into account the importance of real-life problem-solving including how to manage real-life stressors when they arise. The presentation will cover key PST principles and tools that can be used in everyday life.Evidence Based Practices Workshop 2 Behavioral Interventions for Stress Management
There are many evidence-based techniques that are easy to learn and practice, with good results in individuals struggling with physical and mental health challenges. This workshop with briefly introduce participants to some of the more common and effective practices including progressive muscle relaxation, guided imagery, diaphragmatic breathing, relaxation response, and mindfulness-based stress reduction. Speakers: Shannon Robinson, MD (HMA), Marsha Johnson, MSW, LCSW (HMA)Problem Solving Worksheet
This worksheet guides the clinician and person receiving services in following the seven steps of problem-solving: Identifying the problem Describing the goal Brainstorming solutions Evaluating the pros and cons for each potential solution Choosing the preferred solution Creating a detailed action plan Evaluating the outcome.Relaxation Handout
This patient-facing handout reviews basic steps for meditation, deep breathing, progressive muscle relaxation, and imagery. This can be used when explaining stress reduction techniques to patients.Evidence Based Practices Workshop 1 Cognitive Behavioral Therapy
Viewing Time 1 Hour
Adapting Evidence Based Practices for Integrated Care
This webinar workshop series focuses on key elements of evidence-based practices/treatments to assist providers with achieving successful implementation and outcomes. HMA presenters discuss key components of EBPs including but not limited to training, indicated populations, fidelity assessments, tools, and other relevant topics. This webinar includes an interview with psychologist Jennifer Frey who discusses the ways in which she uses and adapts the EBP of Motivational Interviewing in her work as a behavioral health consultant at Unity. Following this webinar, there is a series of three EBP workshops that includes cognitive behavior therapy, behavioral interventions for stress management trauma-informed care, problem-solving therapy.Integrated Care DC Provider Information Session
Integrated whole-person care has been shown to improve outcomes and increase Medicaid beneficiary satisfaction. We want to support you to enhance your practice’s capability to deliver person-centered care, use population health analytics, and engage leadership to support value-based care. Join us to learn more about provider engagement opportunities for year 2 of the Integrated Care DC Program.TeleHealth Workflow Comparison
Pregnancy and Substance Abuse: A Harm Reduction Toolkit
This toolkit was designed to help community providers care for pregnant and parenting people who use drugs in a holistic manner. The kit includes information about stigma reduction, trauma-informed care, and legal services. While the guide was developed IN NY, there are engagement and other information that is useful regardless of location.Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
SAMHSA supported the development of this guide in 2018 to promote evidence-informed care for pregnant and parenting women who have OUD. It includes modules on prenatal care, postnatal care, infant care, and more.
Telehealth in a Post-Pandemic Era Sustainable Approaches to Support Integrated Care – Part 2
This interactive virtual workshop is part two of a two-part series to support providers ongoing efforts to implement and sustain innovative models of telehealth following the COVID-19 public health emergency. Topics include best practices to support behavioral health care delivery through telehealth; improving patient engagement through telehealth and DC telehealth policy and priority updates.
Telehealth in a Post-Pandemic Era: Sustainable Approaches to Support Integrated Care – Part 1
https://www.integratedcaredc.com/wp-content/uploads/2021/08/Webinar-Telehealth-in-a-Post-Pandemic-Era-Sustainable-Approaches-to-Support-Integrated-Care.mp4 Webinar This interactive virtual workshop is part one of a two-part series to support providers ongoing efforts...Using Disease Registries to Improve Your Practice Population’s Health
This webinar focuses on effective strategies for engaging justice-involved populations and ways to support individuals transitioning to communities. The speakers shared case studies to illustrate the ways that providers have managed transitions of care and supported people. This session is approved by the American Academy of Family Physicians for up to 1 AMA Level 1 CME credit.Common Comorbidities with Substance Use Disorders Research Report
When two disorders or illnesses occur in the same person, simultaneously or sequentially, they are described as comorbid. Comorbidity also implies that the illnesses interact, affecting the course and prognosis of both.1,2 This research report provides information on the state of the science in the comorbidity of substance use disorders with mental illness and physical health conditions.Promoting Culturally & Linguistically Effective Screening Techniques
This module discusses the importance of employing culturally and linguistically effective strategies when r conducting screening and assessments.Staff Wellness & Support Strategies
This module seeks to highlight strategies that may support staff wellness and retention.Addressing Burnout and Resilience
Burnout is common in healthcare and has increased during the Covid 19 pandemic. This brief presentation defines burnout and it's consequences. Building resilience is a strategy to reduce and prevent burnout. The presentation defines resilience and provides tips in increase personal resilience and organizational resilience.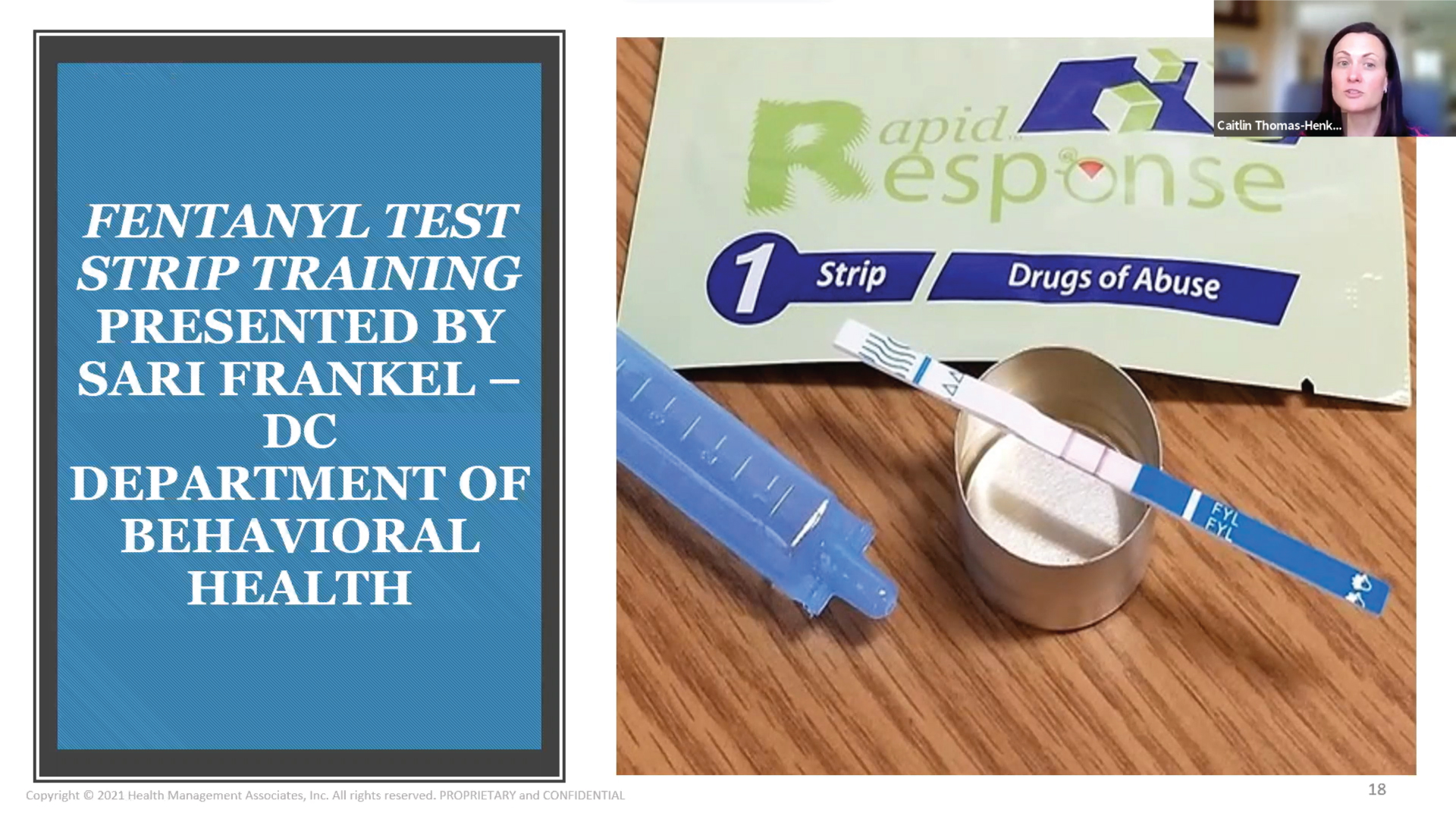
Fentanyl Strip Testing
This brief video provides an overview of fentanyl strip testing to identify the presence of fentanyl in unregulated drugs for people who use drugs (PWUD). It also includes a brief demo of how to use fentanyl test strip testing to detect the presence of fentanyl in their drug supply. Testing for fentanyl test strips can identify the presence of fentanyl in unregulated drugs. They can be used to test injectable drugs, powders, and pills. Being aware if fentanyl is present allows people to implement appropriate harm reduction strategies to reduce the risk of an overdose. Presented by Sari Frankel, DC Department of Behavioral Health.Using Registries for Population Health
Registries are important population health tools that allow organizations to collect, organize, aggregate, and utilize the information for a variety of purposes. Maintaining registries for certain disease states such as depression or diabetes provides easy access to results, identification of care gaps, and level of improvement and can lead to adjustments in care as needed. This Short Take video provides an introduction to registries and how to use them.Mother & Baby Substance Exposure Toolkit
An online resource to provide broad access to resources to clarify best practices to support and improve the care for substance-exposed mothers and newborns. The toolkit includes resources to support screening, assessment, and level of care determination; treatment; transitions of care; and education.Addiction Free California
The California Department of Health Care Services (DHCS) has implemented the California Medications for Addiction Treatment (MAT) Expansion Project to address the opioid epidemic throughout the state. This website serves as a separate yet complementary resource to the DHCS MAT Expansion Website and provides resources and information related to the four MAT Expansion Project initiatives operated by Health Management Associates. The California MAT Expansion Project aims to increase access to MAT, reduce unmet treatment need, and reduce opioid overdose-related deaths through the provision of prevention, treatment, and recovery activities. The project focuses on individuals experiencing homelessness, youth, rural, and tribal populations with limited MAT access. The California MAT Expansion Project, composed of nearly 30 initiatives, is funded by grants from the Substance Abuse and Mental Health Services Administration (SAMHSA).HMAedu – A Learning Management System for Treatment Teams
HMAedu.com is an educational resource specifically designed for training treatment teams about addiction, pain, and behavioral health. With over 25 hours of education through the lens of patient-centered care, users can explore topics of interest or follow the suggested curriculum path. Once a user signs in, the learning management system automatically loads modules that are pertinent to the user’s level of training. This automation allows for consistency in messaging to all providers without delivering information beyond the scope of practice. Each course starts with a TED Talks-style overview that is followed by patient-focused modules of 3-10 minutes each. Each module is traced for completion and can be reported back to the client and individual for tracking purposes.Effective Strategies to Enhance Transitions of Care for Justice Involved Populations
This webinar focuses on effective strategies for engaging justice-involved populations and ways to support individuals transitioning to communities. The speakers shared case studies to illustrate the ways that providers have managed transitions of care and supported people. This session is approved by the American Academy of Family Physicians for up to 1 AMA Level 1 CME credit.Brief Interventions Part 2: Behavioral Activation & More
This brief webinar will review the basics of behavioral activation, distress tolerance skills, and problem-solving therapy to use in skills-based, time-limited treatment settings.Brief Interventions Part 1: Motivational Interviewing & Mindfulness
This brief video introduces the concept of brief interventions and review motivational interviewing and mindfulness. Presented by Dr. Lori Raney, Principal, Health Management Associates.The Process of Enhanced Referral
This brief video explains the process of enhanced referral to improve patient engagement and completion of the referral and improve provider relationships with referrals. Presented by Dr. Lori Raney, Principal, Health Management Associates.Quick Guide: Building Partnerships to Enhance Care Coordination
This is a short reference guide to developing a structure to enhance the referral experience for providers and service recipients. It covers setting standards for partnership starting with your value proposition. It outlines the continuum of provider relationships from informal agreements through forming a business entity and finally provides initial guidance and further resources for establishing care compacts.
Best Practices in Videoconferencing-Based Telemental Health
This document represents a collaboration between the American Psychiatric Association (APA) and the American Telemedicine Association (ATA) to create a consolidated update of the previous APA and ATA official documents and resources in telemental health to provide a...Dimensions: Tobacco Free Toolkit for Health Care
The toolkit contains a variety of information and resources including a step by step guide about: education about tobacco use skills for engaging people in tobacco cessation discussions efficient methods for assessing readiness to quit information and research on treatmentsPeers Speak Out: Priority Outcomes for Substance Use Treatment & Services
The research presented by these three groups seeks to prioritize desired treatment outcomes as defined by diverse people with lived experience. From this information, the researchers crafted recommendations that could help policymakers, providers and researchers develop, implement, reimburse and evaluate more engaging and perhaps effective substance use services.Core Competencies Framework for Practice Transformation
The goal of the ICTA program is to improve care and Medicaid beneficiary outcomes within three practice transformation core competencies: Delivering person-centered care across the care continuum Using population health analytics to address complex medical, behavioral health, and social needs; and Engaging leadership to support value-based care. This document provides more detail, including sub-elements for each core competency.
Harm Reduction 101: Harm Reduction Basics and Lessons From the Field
People with substance use disorders are at particular risk for overdoses and developing one or more primary conditions or chronic diseases. During this webinar, presenters will discuss harm reduction as a public health approach that aims to reduce harms related to substance use. Presenters will discuss strategies, policies, programs, and practices that aim to minimize negative health, social and legal impacts associated with drug use, drug policies, and drug laws.
Understanding Harm Reduction: Substance Use
A documented overview of harm reduction, including definitions, benefits related to substance use, and frequently asked questions.Opioid Overdose Prevention ToolKit
This toolkit provides safety advice for patients and family members to help prevent overdose and how to safely use naloxone.Clinical Use of Extended-Release Injectable Naltrexone in the Treatment of Opioid Use Disorder: A Brief Guide
This document contains information about assessing the need for treatment; initiating MAT; monitoring patient progress and adjusting treatment plan; deciding whether and when to end MAT.Common Questions and Concerns about Medication Assisted Treatment (MAT): A Handout for Ambivalent Patients
This document consists of common questions and concerns about Medication Assisted Treatment for Ambivalent patients. This document can be used as a starting point to have conversations with your patients. In the end, the patient will be able to make an informed decision that’s in line with their values and hopes for recovery.Common Questions & Concerns About MAT: A Handout for Family Members of a Person with OUD
This question and answer document answers common questions and concerns that family members have about Medication Assisted Treatment (MAT). The purpose of this document is to assist providers in educating family members.Early Recovery Tips for Patients
Patients can use this Early Recovery Handout to determine behaviors when cravings or urges arise or behaviors have changed. The document provides strategy to mitigate any behavioral outliers while keeping the patient on track from day to day.The Next Stage of Buprenorphine Care for Opioid Use Disorder
This article reviews research findings in the following 7 areas: location of buprenorphine induction, combining buprenorphine with a benzodiazepine, relapse during buprenorphine treatment, requirements for counseling, uses of drug testing, use of other substances during buprenorphine treatment, and duration of buprenorphine treatment.Pocket Guide: Medications for Addiction Treatment of Opioid Use Disorder SAMHSA
The Medication-Assisted Treatment Of Opioid Use Disorder pocket guide to provide guidance on how to assess the need for treatment, referring to higher levels of care if necessary and the approved frequency and route of administration for treatment of Opioid Use Disorder. In addition, a tool has been provided to determine clinical opiate withdrawal.FAQs for OUD Prescribing and Dispensing in COVID 19 Emergency
The frequently asked questions document discusses how providers can provide Opioid Treatment to existing and new patients, and dispense medications via Telehealth while still meeting the 42 C.F.R. 8.11 requirements.Providing Culturally Sensitive, Patient Centered Care
During the webinar, the presenter will focus on ways to address health equity issues and key considerations for providing linguistically effective services. The presenter will discuss best practices and models to support patients in these challenging times.Understanding the Brain and Treatment for People with Opioid Use Disorders
Understanding the brain chemistry associated with opioid use disorder treatment is essential: Medications for Addiction Treatment (MAT) restores depleted dopamine in the brain so people impacted by OUD can regain functioning. Recognizing this, therapy and support services for OUD are most effective when provided in accordance with a person's healing process and readiness to engage in treatment.Substance Use Disorders: Screening and Assessment
The American Society of Addiction Medicine (ASAM) has established specific criteria for patient assessments and level of care determinations pertaining to substance use disorder (SUD) – providing the underpinnings for effective treatment and recovery from addiction. This webinar will provide attendees with practical tools and tips for implementation of Screening Brief Intervention and Treatment (SBIRT) including assessments, workflows, and reimbursement.Stigma, Myth Busters & Engagement Strategies
This webinar will describe how stigma impacts perceptions and resultant SUD care for patients and providers alike. Presenters will also share key concepts and case studies to illustrate ways to address stigma and tools that can be incorporated into their clinical practice.Integrated Physical and Behavioral Healthcare 102
This webinar will focus on the benefits and outcomes of behavioral health integration and key implementation considerations. The presenters will discuss outcomes that include improving population health, patient experience and reduced costs. The webinar will also feature key integration tips such as building internal support, warm handoffs, establishing workflows among other topics.