Strategies For Effective Quality Improvement In Value Based Arrangements – Cost of Care Part 4
Description: This webinar explores the critical connection between the cost of healthcare services and quality outcomes. Attendees gained the skills to identify a set of meaningful metrics to monitor that inform strategic opportunities to elevate the quality of care...
Understanding Cost of Care to Drive Value-Based Payment Arrangements – Cost of Care Part 3
Description: It is important for healthcare providers to understand the cost of the services they provide and compare that to reimbursement rates. In value-based care arrangements, they should also anticipate the impact of their care models on patient outcomes and...
Decoding Healthcare Finances Understanding Costs And Indirect Allocation Strategies Cost of Care Part 2
Description: With the District of Columbia’s movement to a reimbursement system with services defined and paid through a procedure code, health care leadership must understand the costs that are directly provided and those that indirectly support the service....
Supporting Practice Leaders Navigating Unfamiliar Waters – Leadership Through Change
Practice leaders face more decisions than ever as the District of Columbia works to build an integrated health system that delivers whole person care. This learning series is designed to help organizational decision makers better manage change within a dynamic health system. Part 1 will introduce ways that leadership can transform ingrained policies and practices using new information, data points, and approaches to improve care access and outcomes. The session will also preview exciting next steps for the learning series moving into 2024.
Developing Your Value Based Payment (VBP) Value Proposition
In the dynamic landscape of healthcare, crafting a compelling value proposition involves a strategic blend of audience understanding, innovation, and responsiveness to the needs of payers, community partners and other stakeholders. This short take describes the steps to creating a strong value proposition.
Value-Based Payment (VBP) Virtual Learning Collaborative
Transitioning to payment models that support value-based care means doing business differently. Many District healthcare providers are requesting assistance preparing for and implementing this important change. This virtual learning collaborative focused on legal agreements, contracting, and financial topics, including revenue cycle management and assessing risk. Presenters shared scenarios, assessments, and tools to advance capacity and understanding.
How to Negotiate Your Share with Payers
This short take video will outline the elements of shared savings contract and where the “share” fits in. It will outline some of the key considerations to think about when trying to negotiate your share of savings with a payer for a value-based contract (including downside risk v. upside potential, contract structure, and other value-based care funding), as well as touch on internal considerations for providers when negotiating a share of savings (i.e. is the share enough to cover the provider’s investment to perform in the contract).
Key Considerations for Value-Based Payment (VBP) Arrangements
Value-Based Payment (VBP) arrangements with MCOs are generally described in a separate exhibit to a provider's managed care contract. This session will help participants assess the opportunities and risks of participating in VBP arrangements by evaluating legal terms associated with pay-for-performance programs, total cost of care programs, and capitation payment arrangements. Finally, the session will offer participants practice pointers for evaluating contract terms and examples of favorable and unfavorable VBP contract terms.
VBP Medicaid Managed Care Term Sheet
This tool helps FQHCs understand all of the various VBC elements that are encompassed in a model or program and can impact performance and hence are important consideration in the contract analysis. It provides the considerations, but also guidance on how to approach them and what may be favorable or unfavorable terms within a contract, depending on the scenario and LAN category.
Value-Based Payment: Is it Disrupting Health Care for the Better? Role of a Clinically Integrated Network – FQHC Part 3
Medicare, state Medicaid agencies, managed care organizations, and commercial insurers are increasingly adopting value-based payment (VBP) models. Community Health Centers (CHCs) are uniquely positioned to deliver on that high expectation by offering enhanced access to high quality primary care, coordinating the care delivered by specialists, hospitals and other institutions and care managing the most complex individuals. This requires CHCs to transform their care delivery to efficiently deliver optimal patient- and population-level health outcomes and successfully manage costs. Many CHCs are forming clinically integrated Networks to create contracting leverage, make joint investments in data analytics and collaborate to develop complex care management and clinical models of care.
Understanding Your Clinic’s Current Strengths & Potential in the Context of DC’s Medicaid MCOs’ Legal Obligations to DHCF
https://www.integratedcaredc.com/wp-content/uploads/2023/09/Understanding-your-clinics-current-strengths-and-potential-in-the-context-of-DCs-Medicaid-MCOs-legal-Obligations-to-DHCF.mp4 Description: Community-based providers often possess competitive advantages...
RAG Tool for Quality Measures and Contracts
https://www.integratedcaredc.com/wp-content/uploads/2023/09/RAG-Tool-for-Quality-Measures-and-Contracts.mp4 Description: RAG is a tool designed to assess the viability of expectations related to quality metrics and reporting requirements providers may encounter...
Clinical and Programmatic Implications of VBP – VBP Foundations Part 4
https://www.integratedcaredc.com/wp-content/uploads/2023/09/Clinical-and-Programmatic-Implications-of-VBP-.mp4 Description: Value-based payment reimbursement links payment to the quality and effectiveness of care we deliver. This webinar considers the clinical...
Managing High Cost High Need Individuals – Behavioral Health VBP Part 4
High-need, high-cost (HNHC) patients often face multiple challenges including high disease burden, behavioral health comorbidity, functional limitations and social barriers to treatment plan compliance. They typically make up just 5 percent of the population, but account for 50 percent of health care costs. This webinar will discuss taking a tailored approach to care in order to improve their outcomes.
Allocation of Value-Based Payment Incentive Payments to Optimize Performance – VBP Foundations Part 3
One of the greatest threats to success for clinically integrated networks is an uneven commitment from disparate providers to improve patient outcomes and reduce avoidable, low-value healthcare costs. Success depends on providers investing time and other resources to achieve performance targets. Although the distribution of value-based payments should certainly take into consideration the number of patients either attributed or served, it must also recognize the contribution each entity made to generate the incentive payments. This webinar will explore principles and examples of distribution methodologies aimed at fairly allocating those dollars.
Risk Mitigation and Risk Reserves
https://www.integratedcaredc.com/wp-content/uploads/2023/09/Risk-Mitigation-and-Risk-Reserves.mp4 Description: Once health care providers have demonstrated the ability to reach quality performance targets and generate surplus in a shared savings pool, they may...
Data-Driven Insights to Advance Behavioral Health Quality – VBP Foundations Part 2
Advances in digital technologies and data analytics have created unparalleled opportunities to assess health data accelerating the ability of science to understand and contribute to improved health behavior and health outcomes. Additionally, behavioral health in the United States is being challenged to address persistent health inequities while improving the quality and value of the care delivered. As regulators, payors, and policies push behavioral health toward data-driven performance, the pressure for behavioral health providers to measure and monitor outcomes increases. This training will introduce providers to the key facets of using data to drive performance including metric selection, diagnosing performance issues and acting on data, driving innovation, and making data analytics a central part of the behavioral health quality strategy.
Accountable Care Organization (ACO) Fundamentals
A basic overview of the structure and function of Accountable Care Organizations (ACO) as well as an exploration of their challenges and opportunities in advancing value based care contracts with the government and private payers.
Value-Based Payment: Is it disrupting health care for the better? Role of a Capitated Alternative Payment Model – FQHC Part 2
This webinar will focus on the “why” of transitioning from fee-for-service to capitation to pay for community health center direct services. Dr. Jones will discuss how fee-for-service reimbursement limits patient access to care and hampers efforts to improve patient self-management and accountability for their own health. He will share examples of how innovators are using lessons learned from other service industries to disrupt the health care market. Participants will learn how moving away from the fee-for-service system can preserve revenue streams but also support new models of care, and how payment reform can help to address primary care workforce shortages.
Understanding Key Terms in Managed Care Contracts – VBP Legal Training Part 2
Managed care contracts, like many legal contracts, are challenging to understand. This session will provide a roadmap to key terms commonly found in managed care contracts. The session will explain what these terms mean in plain language and offer examples of favorable and unfavorable terms. In addition, the session will offer pointers for evaluating the favorability of contract terms and describe potential changes to standard terms that participants may wish to address during negotiations.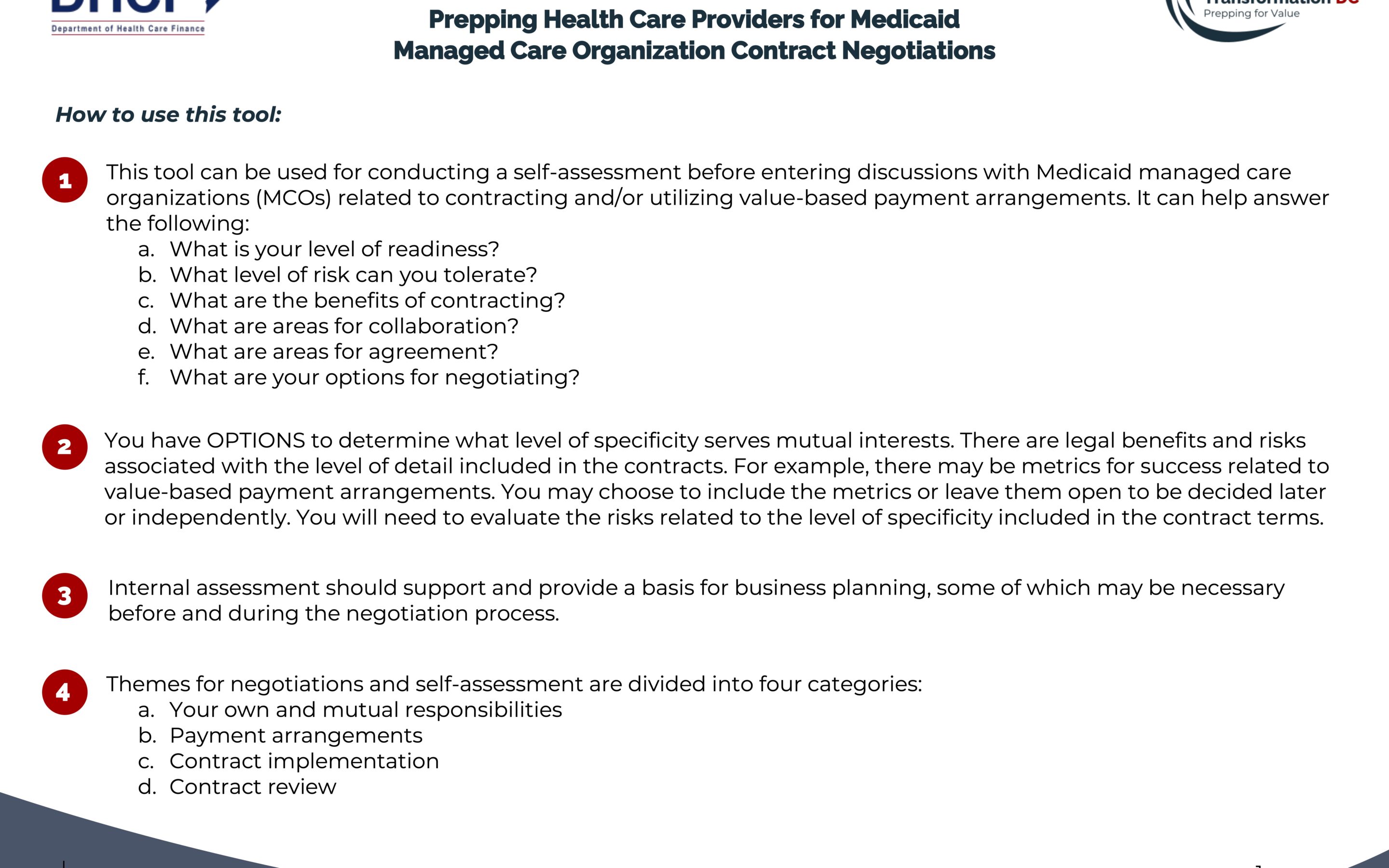
Health Care Provider Checklist for Entering into Managed Care Contracts
This is a self-assessment tool intended to help health care providers plan for negotiations around proposed managed care contracts. The tool can be used for internal conversations to analyze key terms, develop strategic direction, and set priorities for approaching negotiations. This tool can help providers determine if they are ready to contract, what level of risk they can tolerate, and what areas to focus on in negotiations.
Value-Based Purchasing 101: The “Basics” – VBP Foundations Part 1
An introduction to the basic concepts, structures, models, and mechanics of value-based payments.
Clinically Integrated Networks: Build, Buy or Stay on the Sidelines – FQHC Part 1
CMS has signaled its intent to move from strict fee-for-service reimbursement to value-based payment for Medicaid as it has been actively doing for Medicare over the past decade. A few FQHCs are pursuing advanced alternative payment models on their own but most are choosing to clinically integrate with others, especially other FQHCs. This session will share national experiences from these initiatives and provide a framework for evaluating strategic options for DC FQHCs to progress in their pursuit of advanced alternative payment models.
Strategies for Negotiating Managed Care Contracts – VBP Legal Training Part 1
This is a self-assessment tool intended to help healthcare providers plan for negotiations around proposed managed care contracts. The tool can be used for internal conversations to analyze key terms, develop strategic direction, and set priorities for approaching negotiations. This tool can help providers determine if they are ready to contract, what level of risk they can tolerate, and what areas to focus on in negotiations.
LGBTQ+ Cultural Competency Training – Part 2
https://www.integratedcaredc.com/wp-content/uploads/2023/06/LGBTQ-Cultural-Competency-Training-Part-2.mp4 Description: Lesbian, gay, bisexual, transgender, and questioning/queer (LGBTQ+) individuals are frequently underserved and experience significant...
Integrated Care DC Managed Care Readiness Workshop
View materials from this event hosted by Department of Health Care Finance, DBH Training Institute, & Integrated Care DC on May 9, 2023. The in-person workshop was designed for behavioral health providers and other organizations seeking to prepare for the integration of behavioral health into the District’s Medicaid Managed Care Program. Presenters shared information and facilitated exercises to help leadership, clinical and operational staff, and other stakeholders develop the organizational competencies needed to succeed in managed care, including an understanding of managed care principles, how to communicate effectively with managed care partners, and how to effectively demonstrate the value of care through quality measurement and population health.
LGBTQ+ Cultural Competency Training Part 1
Lesbian, gay, bisexual, transgender, and questioning/queer (LGBTQ+) individuals are frequently underserved and experience significant disparities in health outcomes and accessing preventive and ongoing healthcare. Sexual and gender minorities (SGM) often experience discrimination and bias in health care settings and may delay or avoid medical and preventive care. Developing safe, culturally competent healthcare environments and practices for LGBTQ+ patients is critical and closely related to individuals’ willingness to openly share their sexual orientation and/or gender identity and expression (SOGIE). Capturing SOGIE data is critical as it allows providers to have a more comprehensive picture of key factors that influence care. This session will start with a brief discussion of SOGIE terminology and a compilation of what is known about medical and behavioral health needs and disparities among the LGBTQ+ community. We will highlight the critical need for creating environments that improve patients’ psychological safety and increase their willingness to share SOGIE characteristics. We will share examples of how this data could be utilized to improve care and patient satisfaction, including capturing a patient’s preferred name and pronouns, and ways to engage in respectful conversations that could reveal key aspects of their medical history that could otherwise go unnoticed.
Dosing and Titrating Care (PCBH Series Part 10)
A core skill in caring for patients in primary care is the ability to dose and titrate care for individual patients in a way that produces quality outcomes for the patient and allows a provider to care for populations of patients effectively. This session will increase the mindfulness and skills clinicians employ for dosing and titrating care from within the PCBH model.Addressing Grief in PCBH (PCBH Series Part 9)
Loss and grief are common and often come up during primary care encounters. Grief can be caused by separations, incapacity, bereavement, migration, job loss, birth, retirement, or professional loss. We will focus on addressing grief related to the loss of a loved one in this webinar. One-third of people affected by loss can experience physical or mental health problems, such as increased risk of heart disease, suicide, psychosomatic disorders, and psychiatric issues. However, loss can also lead to personal growth. Behavioral Health Consultants can help PCPs and patients prepare for grief and build coping skills for better health outcomes.
Treatment Planning (Quality & Population Health Series, Part 2)
We often think of the treatment plan as a document to complete. However, it can be a tool to engage and empower the person served in their own recovery process. In this interactive webinar we will learn the core components of the treatment planning process from a person-centered and engagement-focused lens.
Guiding: Using Motivational Interviewing Skills to Guide Conversations (Motivational Interviewing Series, Part 2)
There are three main approaches to helping people make a change, directing, following, and a middle-of-the-road approach of guiding. Motivational Interviewing (MI) promotes guiding as an approach to discovering and uncovering an individual’s motivations, concerns, values, and options. This refresher workshop will provide the opportunity to directly practice using MI skills to build discrepancy and move conversations towards enhancing commitment to change.
Quality Measurement Basics: And Why it Matters (Quality & Population Health Series, Part 1)
Understanding, measuring, working to improve quality performance are critical to ensuring that patients have positive outcomes and providers are satisfied—they’re also critical to ensure your practice is meeting its regulatory requirements and maximizing payment opportunities. As the District of Columbia carves in behavioral health care to managed care arrangements and requires more providers to be in value-based care arrangements, it is even more imperative that quality measurement and improvement is understood and infused across your organization—from providers, to leaders, to auxiliary staff. This two-part series will describe the quality measurement basics and why it matters, and then treatment planning for population health. In Part 1, we will explore why we need to infuse a culture of quality within healthcare organizations, including an understanding of what we value, who we serve, and who we are accountable to. Presenters will emphasize the importance of all staff understanding quality and its impact on our patients, staff and organization. We will review the basics of measurement and key measures in quality focused on integrated care.Is a 20-minute consultation realistic? (PCBH Series Part 8)
In making the transition from practicing outpatient behavioral health to primary care behavioral health, clinicians often wonder, how can I do my work in 20 minutes, and is it really possible to make a meaningful difference in this amount of time? This training answers this question directly by simulating a 20 minute behavioral health consultation and discussing as a group each stage of the encounter, best practices, and the strengths and challenges that arise.
Motivational Interviewing Refresher: Using Open Ended Questions, Affirmations, Reflection & Summarizing (OARS) Skills to Strengthen Motivation to Change (Motivational Interviewing Series, Part 1)
In this first workshop, will spend the majority of the time directly practicing foundational OARS skills to evoke interest and commitment to making health behavior changes.Sustainable Trauma Treatment: How Accelerated Resolution Therapy can be Utilized in a PCBH Setting to Effectively Treat Trauma (PCBH Part 7)
Evidence-based modalities developed to treat trauma are commonplace in outpatient behavioral health practices, but we often struggle to adapt these therapies to the integrated care setting where brief intervention is common. In this session, we will present Accelerated Resolution Therapy (ART) as a useful tool for treating trauma in an integrated setting. Accelerated Resolution Therapy has been shown to achieve benefits rapidly, usually within 1-5 sessions, and is effective in treating PTSD and complex trauma as well as other mental health problems such as anxiety, depression, phobias, grief, chronic pain, and relationship issues. We will explore the basics of Accelerated Resolution Therapy, highlight examples of how it has been used effectively in the primary care setting, and discuss both benefits and barriers to implementing this modality. We will focus on the compatibility of this therapy as a brief intervention within the PCBH model and the particular benefit of sustainability as Accelerated Resolution Therapy reduces exposure to vicarious trauma – critical to clinician self-care and preservation in these trying times.Allowing Data to Tell a Story: Relevant Metrics to Help Reflect the Infinite Values of Integrated Healthcare (PCBH Part 6)
As healthcare centers around the country further embrace data and metrics, integrated primary care behavioral health programs must incorporate data to reflect the value of work being done. In this webinar, attendees will learn about primary data and metric points and the importance of ensuring that data tells a story and reflects the infinite values of health systems, rather than becoming finite goals.
Achieving Better Outcomes Through Value-Based Care & Population Health Strategies (LAN Framework Part 2)
During this webinar, presenters discussed how proactive approaches to value-based care, including the use of VBP models, can improve individual and population health outcomes while enhancing efficiencies and reducing total costs. We also featured AmeriHealth’s new care coordination dashboard focused on helping providers close care gaps and achieve better patient outcomes.Behavioral Health Consultation: Handling Behavioral Health Emergencies in Primary Care (PCBH Part 5)
Managing emergencies is challenging in a high-volume, fast-paced environment. This webinar addresses the ways that BHCs and the primary care team can effectively and efficiently address emergencies.Viewing Time 60 Minutes
Understanding Value-Based Care & Value-Based Purchasing (LAN Framework Part 1)
During this webinar, participants will be able to identify the foundations of value-based care and the Health Care Payment Learning & Action Network (HCPLAN or LAN) value-based payment (VBP) framework. The presentation will also include the Department of Health Care Finance’s VBP strategy.It’s a Matter of Context & Compassion: Utilizing Contextualism to Promote Engagement and Health Behavioral Change (PCBH Part 4)
The session will address the realities of health behavioral change and subsequent adherence in integrated, primary care settings, and key lifestyle interventions and recommendations that transcend many evidence-based guidelines for chronic conditions (e.g., diabetes, hypertension, etc.). The session will discuss the importance of filtering evidence-based medicine guidelines through the prism of contextual and compassionate healthcare to increase the probability of patients embracing and implementing such interventions.
From Beginning to End: A Case-Based Experiential Session About Advance Care Planning (Advance Directive & Person-Centered Care Planning Series 3)
This case-based, hands-on session will allow physical and behavioral health professionals to walk through the steps of engaging patients with different presentations and personalities in Advance Care Planning, codifying their wishes in Advance Directives, and making those Advance Directives accessible on the health information exchange. The session’s experiential design will help providers consolidate their skills, increase their comfort and confidence, and feel inspired to approach patients about Advance Care Planning with new ideas and tools. It will include ad hoc case discussions and time for providers to raise questions and concerns.Making Brief Interventions Radical: Infusing focused Acceptance & Commitment Therapy Integrated Primary Care (PCBH Part 3)
This webinar discusses the concept of functional contextualism and the impact this philosophy has on the therapeutic orientation of focused Acceptance and Commitment Therapy (fACT). Specifically, the session will present fACT concepts such as the Contextual Interview, philosophical underpinnings, and influences of psychological flexibility. The session will also cover the philosophy of functional contextualism/fACT fits well within the Primary Care Behavioral Health philosophy.
Overcoming Patient Reluctance & Provider Discomfort to Engage in Advance Care Planning (Advance Directive and Person-Centered Care Planning Series 2)
Among the many barriers to Advance Care Planning, patient reluctance and provider discomfort play large roles. In this highly interactive workshop, we’ll discuss concrete behavioral strategies for overcoming the fears that prevent patients from planning for end-of-life care or times when they are incapacitated. Specific topics include employing the spirit of Motivational Interviewing, normalizing doubts, and helping patients understand the benefits for their family members when they decline to plan. The importance of codifying patient wishes and uploading them to health information exchanges through AD Vault will be stressed. Case illustrations will be used throughout.
Effective Utilization of CRISP DC For Care Coordination By Outpatient Behavioral Health Providers (DCHA Transitions of Care 2)
Representatives from CRISP DC demonstrated how to use the platform to improve care coordination for patients across the healthcare system.