Evidence Based Practices Workshop 1 Cognitive Behavioral Therapy
Viewing Time 1 Hour
Pregnancy and Substance Abuse: A Harm Reduction Toolkit
This toolkit was designed to help community providers care for pregnant and parenting people who use drugs in a holistic manner. The kit includes information about stigma reduction, trauma-informed care, and legal services. While the guide was developed IN NY, there are engagement and other information that is useful regardless of location.Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
SAMHSA supported the development of this guide in 2018 to promote evidence-informed care for pregnant and parenting women who have OUD. It includes modules on prenatal care, postnatal care, infant care, and more.Telehealth in a Post-Pandemic Era: Sustainable Approaches to Support Integrated Care – Test
Viewing Time 1 Hour
Telehealth in a Post-Pandemic Era Sustainable Approaches to Support Integrated Care – Part 2
This interactive virtual workshop is part two of a two-part series to support providers ongoing efforts to implement and sustain innovative models of telehealth following the COVID-19 public health emergency. Topics include best practices to support behavioral health care delivery through telehealth; improving patient engagement through telehealth and DC telehealth policy and priority updates.
Telehealth in a Post-Pandemic Era: Sustainable Approaches to Support Integrated Care – Part 1
https://www.integratedcaredc.com/wp-content/uploads/2021/08/Webinar-Telehealth-in-a-Post-Pandemic-Era-Sustainable-Approaches-to-Support-Integrated-Care.mp4 Webinar This interactive virtual workshop is part one of a two-part series to support providers ongoing efforts...TEAMcare An Integrated Multicondition Collaborative Care Program for Chronic Illnesses and Depression
Patients with poorly controlled diabetes, coronary heart disease, and depression have an increased risk of adverse outcomes. In a randomized, controlled trial, we tested an intervention designed to improve disease control outcomes for diabetes and/or heart disease and coexisting depression. Patients with one or more parameters of poor medical disease control (ie, HbA1c ≥8.5, or SBP >140, or LDL >130) and a Patient Health Questionnaire-9 (PHQ-9) ≥10 were randomized to the TEAMcare intervention or usual care (N = 214). This article will describe the TEAMcare health services model that has been shown to improve quality of care and medical and psychiatric outcomes.Principles of Adolescent Substance Use Disorder Treatment: A Research-Based Guide
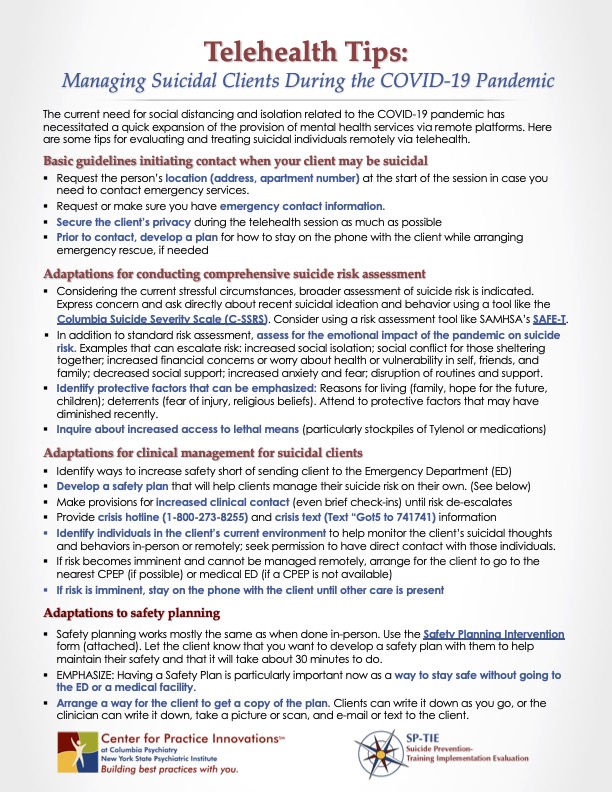
Telehealth Tips: Managing Suicidal Clients During the COVID-19 Pandemic
The current need for social distancing and isolation related to the COVID-19 pandemic has necessitated a quick expansion of the provision of mental health services via remote platforms. This tip sheet provides some tips for evaluating and treating suicidal individuals remotely via telehealth.Information for Behavioral Health Providers in Primary Care: Stages of Change: Key Features
Change is not a concrete process, but rather, a fluid process. Individuals tend to move through different “stages of change” in the management of medical problems. These stages include: 1) precontemplation, 2) contemplation, 3) preparation, 4) action, and 5) maintenance.How to Measure Motivational Interviewing Fidelity in Randomized Controlled Trials: Practical Recommendations
Many randomized controlled trials in which motivational interviewing (MI) is a key intervention make no provision for the assessment of treatment fidelity. This methodological shortcoming makes it impossible to distinguish between high- and low-quality MI interventions, and, consequently, to know whether MI provision has contributed to any intervention effects. This article makes some practical recommendations for the collection, selection, coding and reporting of MI fidelity data, as measured using the Motivational Interviewing Treatment Integrity Code. We hope that researchers will consider these recommendations and include MI fidelity measures in future studies.Telehealth for the Treatment of Serious Mental Illness & Substance Use Disorders
This guide contains a foreword and five chapters. The chapters stand alone and do not need to be read in order. Each chapter is designed to be brief and accessible to healthcare providers, healthcare system administrators, community members, policymakers, and others working to meet the needs of people at risk for, experiencing, or recovering from SMI and/or SUD. The goal of this guide is to review the literature on the effectiveness of telehealth modalities for the treatment of SMI and SUD, distill the research into recommendations for practice, and provide examples of how practitioners use these practices in their programs.Use of the Family CAGE in Screening for Alcohol Problems in Primary Care
To establish the reliability and validity of the Family CAGE (an acronym indicating Cut down on drinking; Annoyed by complaints about drinking; Guilty about drinking; had an Eye-opener first thing in the morning), a four-item instrument intended to assess family alcohol-related problems.
Counseling Patients in Primary Care: Evidence-Based Strategies
Family physicians spend substantial time counseling patients with psychiatric conditions, unhealthy behaviors, and medical adherence issues. Maintaining efficiency while providing counseling is a major challenge. There are several effective, structured counseling...Fighting Back Against the Stigma of Addiction
Untreated drug and alcohol use contributes to tens of thousands of deaths every year and affects the lives of many more people. We have effective treatments, including medications for opioid and alcohol use disorders, that could prevent a significant number of these deaths, but they are not being utilized widely enough, and people who could benefit often do not even seek them out. One important reason is the stigma around those with addiction.Common Comorbidities with Substance Use Disorders Research Report
When two disorders or illnesses occur in the same person, simultaneously or sequentially, they are described as comorbid. Comorbidity also implies that the illnesses interact, affecting the course and prognosis of both.1,2 This research report provides information on the state of the science in the comorbidity of substance use disorders with mental illness and physical health conditions.Advancing Integrated Mental Health Solutions – Collaborative Care Resources
Collaborative Care (CoCM) is a specific type of integrated care developed at the University of Washington that treats common mental health conditions such as depression and anxiety that require systematic follow-up due to their persistent nature. Based on principles of effective chronic illness care, Collaborative Care focuses on defined patient populations tracked in a registry, measurement-based practice, and treatment to target. Trained primary care providers and embedded behavioral health professionals provide evidence-based medication or psychosocial treatments, supported by regular psychiatric case consultation and treatment adjustment for patients who are not improving as expected.Promoting Culturally & Linguistically Effective Screening Techniques
This module discusses the importance of employing culturally and linguistically effective strategies when r conducting screening and assessments.Staff Wellness & Support Strategies
This module seeks to highlight strategies that may support staff wellness and retention.Mother & Baby Substance Exposure Toolkit
An online resource to provide broad access to resources to clarify best practices to support and improve the care for substance-exposed mothers and newborns. The toolkit includes resources to support screening, assessment, and level of care determination; treatment; transitions of care; and education.Addiction Free California
The California Department of Health Care Services (DHCS) has implemented the California Medications for Addiction Treatment (MAT) Expansion Project to address the opioid epidemic throughout the state. This website serves as a separate yet complementary resource to the DHCS MAT Expansion Website and provides resources and information related to the four MAT Expansion Project initiatives operated by Health Management Associates. The California MAT Expansion Project aims to increase access to MAT, reduce unmet treatment need, and reduce opioid overdose-related deaths through the provision of prevention, treatment, and recovery activities. The project focuses on individuals experiencing homelessness, youth, rural, and tribal populations with limited MAT access. The California MAT Expansion Project, composed of nearly 30 initiatives, is funded by grants from the Substance Abuse and Mental Health Services Administration (SAMHSA).HMAedu – A Learning Management System for Treatment Teams
HMAedu.com is an educational resource specifically designed for training treatment teams about addiction, pain, and behavioral health. With over 25 hours of education through the lens of patient-centered care, users can explore topics of interest or follow the suggested curriculum path. Once a user signs in, the learning management system automatically loads modules that are pertinent to the user’s level of training. This automation allows for consistency in messaging to all providers without delivering information beyond the scope of practice. Each course starts with a TED Talks-style overview that is followed by patient-focused modules of 3-10 minutes each. Each module is traced for completion and can be reported back to the client and individual for tracking purposes.Motivational Interviewing In Primary Care
Healthcare systems are in the process of reforming themselves to better meet the needs of people with, or at risk of developing, chronic diseases and long-term conditions. One goal of these efforts is the coproduction of activated, informed, engaged, and motivated patients and citizens.Dimensions: Tobacco Free Toolkit for Health Care
The toolkit contains a variety of information and resources including a step by step guide about: education about tobacco use skills for engaging people in tobacco cessation discussions efficient methods for assessing readiness to quit information and research on treatmentsPeers Speak Out: Priority Outcomes for Substance Use Treatment & Services
The research presented by these three groups seeks to prioritize desired treatment outcomes as defined by diverse people with lived experience. From this information, the researchers crafted recommendations that could help policymakers, providers and researchers develop, implement, reimburse and evaluate more engaging and perhaps effective substance use services.Core Competencies Framework for Practice Transformation
The goal of the ICTA program is to improve care and Medicaid beneficiary outcomes within three practice transformation core competencies: Delivering person-centered care across the care continuum Using population health analytics to address complex medical, behavioral health, and social needs; and Engaging leadership to support value-based care. This document provides more detail, including sub-elements for each core competency.
Harm Reduction 101: Harm Reduction Basics and Lessons From the Field
People with substance use disorders are at particular risk for overdoses and developing one or more primary conditions or chronic diseases. During this webinar, presenters will discuss harm reduction as a public health approach that aims to reduce harms related to substance use. Presenters will discuss strategies, policies, programs, and practices that aim to minimize negative health, social and legal impacts associated with drug use, drug policies, and drug laws.Providing Culturally Sensitive, Patient Centered Care
During the webinar, the presenter will focus on ways to address health equity issues and key considerations for providing linguistically effective services. The presenter will discuss best practices and models to support patients in these challenging times.Stigma, Myth Busters & Engagement Strategies
This webinar will describe how stigma impacts perceptions and resultant SUD care for patients and providers alike. Presenters will also share key concepts and case studies to illustrate ways to address stigma and tools that can be incorporated into their clinical practice.Integrated Physical and Behavioral Healthcare 102
This webinar will focus on the benefits and outcomes of behavioral health integration and key implementation considerations. The presenters will discuss outcomes that include improving population health, patient experience and reduced costs. The webinar will also feature key integration tips such as building internal support, warm handoffs, establishing workflows among other topics.Addiction Neuroscience 101
This module offers a 25-minute video of the neuroscience of addiction as a chronic brain disease presented by HMA’s Corey Waller, MD, MS, FACEP, DFASAM, with emphasis on Opioid Use Disorder (OUD). "This lecture was developed for audiences of all backgrounds to absorb. From patients to nonspecialist docs. The intent was to move people past the preconceived notion that addiction is a moral failing or choice, to the reality that it is a chronic brain disease that creates maladaptive connections in large swaths of the brain. Over the hundreds of lectures, I have given in my career, I have come to realize that running through 30+ articles in a 70 slide PPT does not move people emotionally. But a good story will. The lecture has coalesced into a story form that is much more compelling than digging through the dense science of voxel dysmorphology, BOLD fMRI technology, and all of the structures postulated to drive craving. If I need a custody officer to "get it" or an administrator to understand the concept, I cannot give them the same lecture I would give a psychiatrist, addiction psychologist, addiction doc, or a neurologist."How to Screen and Assess People for Substance Use Disorder
This webinar focused on the appropriate screening and assessments for substance use disorders, including the difference between screening and assessment, brief interventions for substance-related issues, and medications for opioid use disorder.
Health Literacy in a Care Coordination Context
An overview of health literacy, its impact on health outcomes, challenges facing patients, and health literacy resources and tips for communicating with patients.
Strong Patient Engagement Depends on Strong Teams
This webinar includes a refresher on motivational Interviewing, presented tools to strengthen patient engagement and strategies for enhancing and maintaining clinician capacity to work with consistency, presence, and joy in the work.
Successful Patient Engagement with Resilient Practitioners
During this webinar, Dr. Jeffrey Ring, clinical psychologist discussed strategies for effective member engagement and communications.